Hepatitis C
Hepatitis C spreads through blood-to-blood contact and leads to inflammation of the liver, affecting the organ's work. Hepatitis C is highly infectious and can survive outside the body for more than seven days. There is no vaccine, but the virus can be cured. Left untreated, it can lead to liver cancer.
There are about 1000 new cases of hepatitis C in NZ each year, with about 50,000 people living with the virus. Worldwide, about 200 million people have it. In 2021 NZ's Ministry of Health released an action plan aimed at reducing the incidence of hepatitis C nationwide.
Who is at risk?
You're at increased risk of contracting hepatitis C if you have:
Received a tattoo or body piercing using unsterile equipment
Had a blood transfusion before 1992
Lived or received medical treatment in a high-risk country
Been in prison
A mother living with hepatitis C
Injected drugs. This is the most common cause. Even if you've only injected once, you should get tested. Hepatitis C tests may be available from community-based health professionals as well as in GP clinics or hospitals. Please see your GP for further information.
To avoid spreading the virus to others you should:
Cover any open cuts or sores
Clean any blood spillage with household bleach
Avoid sexual practices that may risk blood contact
Not share piercing, tattooing, drug-injecting or snorting equipment, or objects such as razors and toothbrushes that may risk blood contact
Not donate blood.
What are the symptoms?
Many people with hepatitis C have no symptoms. It is often referred to as a silent epidemic because people commonly don't notice any symptoms until 20 or 30 years after infection. Any symptoms that do appear are usually mild and non-specific. The most common symptoms include tiredness (fatigue), joint pain, loss of appetite, nausea and abdominal pain.
How can hepatitis C affect me?
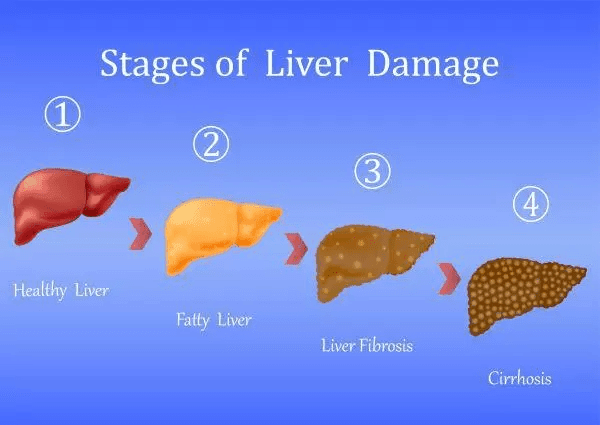
If left unchecked, 20–25 percent of people with hepatitis C will develop cirrhosis of the liver. Of these, 3-5 percent will develop liver cancer each year. Liver damage can lead to liver failure; hepatitis C is the leading cause of liver transplantation in NZ. Of people in NZ with hepatitis C, 50–60 percent remain undiagnosed and unaware of the associated risks.
How can I manage the virus?
If hepatitis C is diagnosed early, you can make lifestyle changes to help delay the onset of serious complications, have treatment and take steps to ensure you don't spread it.
If you experience symptoms such as no energy, low concentration or lack of appetite, you can help yourself by:
Doing some gentle exercises every day
Eating smaller meals
Resting when you feel tired
Having a pre-sleep routine
Not exercising or drinking coffee or tea before bed.
What is acute hepatitis C?
Acute hepatitis C occurs when someone has it for less than six months. One in every three people clear the virus within six months. The others go on to have chronic hepatitis C.
How is hepatitis C diagnosed?
There are two blood tests needed to diagnose chronic hepatitis C.
Antibody test (anti-hepatitis C)
This test checks whether someone has ever been exposed to the virus. It doesn't determine whether the virus is present now or was there in the past. After you have had the virus this test will always be positive, even after you've been cured.
Hepatitis C viral load (HCV RNA)
This test counts the amount of virus particles present in someone's blood. If “not detected” then it means the person does not have hepatitis C. If the virus is present it will give a number (usually 10,000 - 8 million). If the virus is present you should speak to their healthcare provider about starting hepatitis C treatment. This is the main test used in New Zealand to confirm current infection.
HCV RNA/hepatitis C antigen test
This tests looks for virus particles. It will give a positive or negative result. If negative it means the virus isn't present and you don't have hepatitis C. If positive it means the virus is present and you should speak to their healthcare provider about starting hepatitis C treatment. This test does not need to be done if an HCV RNA test has already been done.

Maviret
Find out more about Maviret.
Posters
Get tested, get treated, get cured
Videos/audio
The Hep-cast discusses the road to hepatitis C elimination.



I have hepatitis C. How can I be treated?
Maviret is fully funded for people with hepatitis C. Each tablet has a combination of two anti-viral medicines. Treatment for most people will be three tablets, once a day, for eight weeks, but may need to be for a longer duration if you've been treated for hepatitis C before or have cirrhosis. Please discuss with your healthcare provider how long your treatment course should be. Maviret is effective against all six types (genotypes) of hepatitis C.
Regional district health boards manage hepatitis C patient services. Contact your GP if you think you have hepatitis C or would like to access treatment. If you have questions about hepatitis C or need support please contact us.
If you live in the Central region (the Bay of Plenty, Waikato, Taranaki, Lakes or Tairawhiti), Waikato DHB will manage your monitoring and follow-up. If you have questions about your fibroscan appointment please call Kathryn on +64 7 839 8899 ext: 96289.
If you live in Whanganui, Manawatu, Wairarapa, Hawkes Bay, Wellington, Kapiti and Hutt regions and want to access free screening or help to access treatment get in touch directly with Tū Ora Compass Health by emailing hepcservice@tuora.org.nz or going to http://stickittohepc.co.nz website where there is a list of places in the community offering free screening. They can also help arrange fibroscan testing as indicated
All screening and treatment for HepC can now be accessed free of charge. If you live elsewhere please see your GP for referral to a hepatitis C programme near you.
Liver assessment before treatment
It's important to know how much scar tissue or damage is present. If you have mild or moderate scarring in the liver, your GP can supervise your treatment. After successful treatment, no further follow-up is needed. Scar tissue in the liver will reduce over time.
If severe scar tissue (cirrhosis) is present in the liver, you should be cared for by a specialist clinic. After treatment, you should stay under specialist follow-up because there is a risk of liver cancer (hepatocellular carcinoma), even many years after the virus has been cured.
What happens after treatment?
Being ‘cured’ of the hepatitis C virus means having a sustained virological response (SVR), which is when the virus can't be detected four weeks after treatment.
This is a complete cure from hepatitis C, as being free of the virus three months after treatment means it is unlikely the virus will return. However, you are not immune to hepatitis C and you can be reinfected if you're exposed to the virus again.
If your treatment was successful and your liver is healthy (no cirrhosis), you won't need further follow-up. It is important to maintain a good diet and a healthy lifestyle. Clearing the virus gives your liver time to recover. Your community nurse and/or hospital staff will talk to you about how you can stay healthy.


