Hepatitis and the Liver
Your Liver
The liver is the largest organ in the body. It has more than 500 functions, including fighting infections, filtering waste products, aiding digestion, storing sugar, iron and vitamins to give your body energy, and helping with blood clotting. The liver can also repair itself.
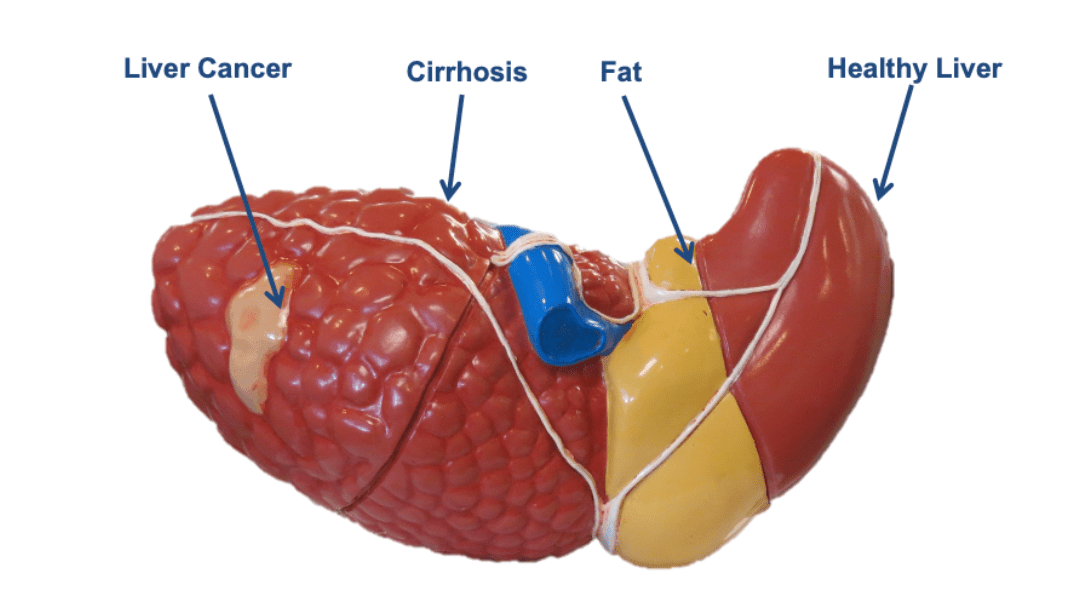
Liver disease can be inherited or caused by damage to the liver from infection, alcohol use and obesity. Over time, this damage can cause scarring (cirrhosis), which can lead to liver failure. This can be life-threatening.
What is hepatitis B?
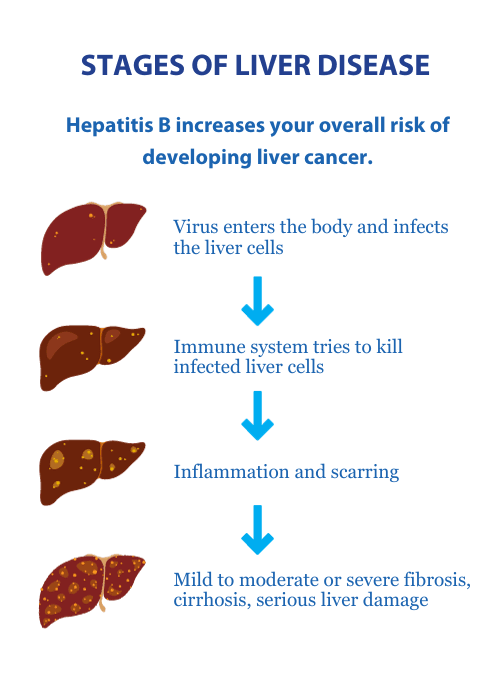
Hepatitis B is a contagious virus which causes damage to the liver.
It's spread through the blood to blood and infected bodily fluids.
Enters the blood and infects the liver.
May lead to serious liver disease including cirrhosis (scarring) or liver cancer.
Chronic hepatitis B occurs if the virus has been in the body for more than six months.
About 100,000 people in New Zealand have it. Adults who acquire hepatitis B can develop an acute illness. They may become sick soon after infection and will usually recover fully, but some can carry the virus in their blood long-term. This can lead to liver damage and liver cancer.
In these cases, lifelong monitoring is needed. If you have hepatitis B, are a New Zealand citizen and are not currently enrolled with us, we invite you to register for free monitoring.
How can it be contracted?
Hepatitis B spreads via blood, semen and other bodily fluids. It is transmitted through:
Contact with infected bodily fluids including dried blood
Unprotected sexual contact with someone who has the virus
Injecting drugs
Receiving a tattoo using unsterile equipment
Hepatitis B can also be transmitted from mother to baby towards the end of pregnancy and during delivery. This is known as vertical transmission and is one of the most common ways people can become infected. Babies and young children who acquire the virus rarely have any symptoms. They commonly go on to have lifelong infections.
You can stop the spread of hepatitis B:
Cover open sores or cuts
Clean any spilt blood with household bleach
Do not donate blood
Don't share razors, or toothbrushes or use unsterilised equipment for drug taking, tattooing, or piercings.
Practice safe sex unless your partner has been immunised.
Know your own status and make sure your whanau are all up to date with routine vaccinations.
What are the symptoms?
Symptoms can include:
nausea
tiredness
dark urine
pale bowel motions
joint and muscle pain
jaundice.
Symptoms appear six weeks to six months after you catch hepatitis B.
Can I get tested and/or vaccinated?
Testing and vaccination should be offered to the household contacts and sexual partners of people who have hepatitis B. Since 1987, all babies born in NZ have been protected against hepatitis B virus infection through vaccination. Find more about the hepatitis B vaccine in New Zealand from the Immunisation Advisory Centre.
Hepatitis B is rare in New Zealanders aged under 25.
Hepatitis B requires long-term monitoring; six-monthly blood tests are vital.
Who do I tell about my diagnosis?
Your hepatitis B test result is personal. You do not have to tell anyone, but you do need to take care not to spread hepatitis B to others.
Hepatitis B is not spread through sneezing, coughing, shaking hands, hugs, kissing, preparing food for others or sharing cooking or eating utensils.
If you have a close family member who has been diagnosed with hepatitis B-related primary liver cancer (HCC), you will require six-monthly ultrasounds, as you may be at a higher risk of liver cancer.
Blood tests are important for people with hepatitis B
They can provide people with the information required to indicate whether treatment is recommended or not. Not everyone needs treatment even though everyone needs monitoring.
Six-monthly blood tests pick up early signs of liver disease such as cirrhosis and liver cancer. Up to 70 percent of your liver can already be damaged by the time you start to feel ill. You may not notice any symptoms from hepatitis B. This is why regular blood tests are important.
What tests do I need?
International guidelines recommend blood tests to monitor the virus and liver are done six-monthly. These tests include:
HBsAg: Hepatitis B surface antigen
HBeAg: Hepatitis B envelope antigen
ALT: screen for active liver inflammation (and possible need for antiviral therapy)
AFP: screen for hepatocellular carcinoma (HCC). This will also be elevated during pregnancy
HBV DNA: measures the amount of virus present in the blood. May be requested every few years.
If repeated blood tests show the ALT level is up and the virus level is high, treatment may be recommended.
Related Links

What to know before your blood test:
Drink plenty of water before the blood test.
You can eat before a blood test.
Make sure you are warm.
Wear a top with sleeves that are easy to roll up.
Have your test as soon as you receive the form.
Tell the nurse if you don't feel comfortable having a blood test.
How can I manage the virus?
Maintaining a healthy lifestyle is important. We recommend daily exercise, avoiding fatty and sugary food and drinks, and keeping your alcohol intake to a minimum. This is one of the most important things you can do to look after your liver. Regular and heavy alcohol intake will increase liver damage, speeding up the progression of liver disease, and raise the risk of cirrhosis.
If you have cirrhosis it's recommended you don't drink at all.
The liver has many important functions and needs to be looked after. Here's how you can love your liver.
Avoid drinking too much alcohol. This is an important part of looking after your liver. Men and women can both get liver damage from too much alcohol. Current recommendations state that women should have no more than two standard drinks a day for women, while men should have no more than three (as a guide, the Health Promotion Agency states a 330ml can of beer at four percent alcohol or one 100ml glass of wine at 12.5 percent alcohol is a standard drink). Both men and women should have at least two alcohol-free days each week.
Exercise and eat well. About 75 percent of obese people have a fatty liver. If you are overweight or obese, gradual weight loss and increasing exercise can reduce your risk of developing a fatty liver.
Stop smoking. Cigarette smoking may worsen some liver diseases and may increase your risk of developing liver cancer. Smoking impairs the liver’s ability to process medications, alcohol and other toxins and remove them from the body.
Get vaccinated. If you're at increased risk of viral hepatitis or you already have any form of liver disease, talk to your doctor about getting the hepatitis A and hepatitis B vaccines.
Practice safe sex. Liver diseases such as hepatitis B and C can be contracted through close physical contact, including sexual intercourse, with someone already affected by the viruses.
Avoid intravenous drug use. This is a common way of contracting hepatitis B and C, especially if you're sharing needles. Sharing personal items such as a toothbrush or razor blade can also transmit hepatitis B and C.
If you need someone other than the Foundation to speak to - where to get help:
Healthline: 0800 611 116
Need to Talk? Free call or text 1737 any time to speak to a trained counsellor, for any reason.
Asian Family Services: 0800 862 342 Monday to Friday 9am to 8pm or text 832 Monday to Friday 9am - 5pm. Languages spoken: Mandarin, Cantonese, Korean, Vietnamese, Thai, Japanese, Hindi, Gujarati, Marathi and English.
Lifeline: 0800 543 354 or text HELP to 4357
Suicide Crisis Helpline: 0508 828 865 / 0508 TAUTOKO (24/7). This is a service for people who may be thinking about suicide, or those who are concerned about family or friends.
Depression Helpline: 0800 111 757 (24/7) or text 4202
Samaritans: 0800 726 666 (24/7)
Rural Support Trust Helpline: 0800 787 254
Rainbow Youth: 09 376 4155
OUTLine: 0800 688 5463 (6pm-9pm)
If it is an emergency and you feel like you or someone else is at risk, call 111.
